TMD, TMJ, Bruxism... USEFUL INFO
Lockdown has been a very challenging time. During these difficult months, many of our patients have presented with broken teeth, restorations and dentures. They often complain about headaches, jaw pain, waking up with clenched teeth and suffer from broken sleep. If you are suffering, you may be exploring TMJ or TMD. Though these two acronyms are often used synonymously, they are quite different. We explain these below as well as treatment options.
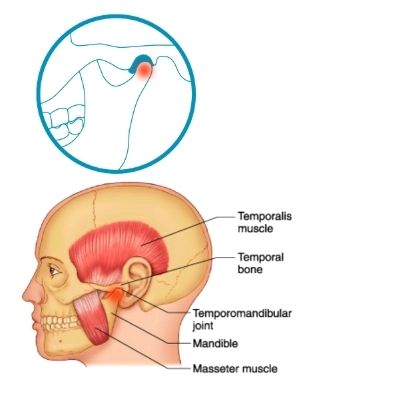
Temporomandibular joint (TMJ)
The temporomandibular joint (TMJ) is the joint that connects the skull with the jaw bone and is located in front of your ear. These two bones are connected by ligaments and muscles, and a joint capsule surrounds the joint.
There is a disc which sits in between the two bones and should move forwards and backwards with the jaw bone as you open and close your mouth. Your TMJs are essential for chewing and talking and are the most used joints in the body.
Temporomandibular dysfunction (TMD)
Temporomandibular dysfunction (TMD) is a collective term for conditions that affect the TMJ or jaw joint and the muscles around the joint.
It is a common condition affecting 8% to 15% (1) of the adult population.
TMD often gets better on its own, but in some cases the pain may last longer and require treatment.
The exact cause of TMD is largely unknown and often no obvious cause can be found. Research suggests that TMD can be caused by a combination of conditions involving the joint, muscles or both. Most of the discomfort associated with TMD may be a result of overuse of the joint and muscles of the jaw.
It is estimated that the TMJ is used over 2,000 times a day in normal functional activity such as talking and eating. However, there are activities which cause an overuse of the jaw, including the following:
- Poor posture. A forward head posture (poking chin) and rounded shoulders will change the way the TMJ functions. Over a period of time, this altered function may cause a problem.
- Clenching the teeth together. This can occur consciously and subconsciously during times of stress, anger, concentration and even in cold weather.
- Grinding the teeth together. This often occurs at night subconsciously. It can also occur during the day and may occur during times of stress.
- Straining the TMJ and its surrounding muscles. This may occur when biting nails, chewing pencils or eating hard or chewy food.
- Overworking the jaw muscles. This may occur with constant chewing, for example chewing gum.
- Stress or concentration. This may cause clenching and grinding, and also holding tension within the facial muscles.
- Habitual playing with piercings. This occurs when tongue piercings or rings are played with, which can cause the jaw to move in potentially awkward positions.
You may experience some of the following symptoms of TMD:
- Clicking, popping or grinding noises coming from one or both of your TMJs during mouth opening. These noises are not always painful. Clicking is a common symptom in the general population who are not suffering with TMD.
- Pain, discomfort or tenderness around the TMJ and surrounding areas, including the muscles.
- Difficulty in opening the mouth.
- Locking when opening or closing the mouth.
- Reduced opening of the mouth.
- Earache or a feeling of ‘fullness’ in the ear.
- Headaches around the temples.
- Neck ache.
- Difficulty with sleeping.
TMD is not a disease. It is usually a temporary dysfunction of the jaw. It can, however, cause irritation. It usually responds well to treatment.
There is some general advice below which is helpful when managing acute pain and longstanding pain. With longstanding TMD, it is common to have flare-ups where you experience a few days or weeks of increased pain and limited mouth opening. This general advice may help you to take control of your TMD:
- Rest your jaw – restrict your jaw movements to daily function activities such as talking and eating.
- Avoid straining your neck and shoulders through poor posture.
- Avoid resting your chin on your hand when leaning your elbow on a table.
- Avoid deliberately pushing your lower jaw forwards to change your jaw position for appearance.
- Consider requesting a workstation assessment to ensure that you are in the best posture while at work.
- Avoid caffeine and smoking. They are stimulants that may excite the nerves in your body which may make your pain appear worse.
- Try to give yourself 10 to 15 minutes each day to relax.
- Avoid clenching your teeth tightly together. This can happen subconsciously, so being aware of this is the first step towards reducing it.
- Identify and avoid oral habits involving biting things which are not food, such as fingernails, skin, lips and pens.
- Eat a softer diet. It is important not to stay on a soft diet for a long time but to gradually return to a normal diet when the pain begins to reduce to its normal level.
- Avoid activities that involve wide opening of the jaw, such as yawning or prolonged dental treatments, until the pain has reduced. You can stifle a yawn or gently put your hand under your chin to prevent full mouth opening when yawning. If you need to have dental treatment within this time, inform your dental practitioner so that prolonged mouth opening can be minimised.
- Apply heat or cold (whichever feels better) on your cheek over the jaw area. It is important to make sure that the heat or cold pack is wrapped in a towel to avoid getting burns on your face. Application time should be limited to five minutes.
- Keep your tongue up in the roof of your mouth and your teeth apart. This helps keep your jaw muscles in a relaxed position.
- Pain reduction medication (analgesia) may help (providing there is no medical reason why you cannot take these).
- Learn and practise relaxation, including abdominal breathing, as this may help during times of increased pain.
- Sleep hygiene (see below for more information).
What is Bruxism?
Bruxism is commonly referred to as grinding the teeth and can occur during the day or at night. If your pain is worse when you wake up, this may be a sign that you are grinding or clenching your teeth at night.
Related Information

Improving your mental wellbeing
We genuinely care about patient wellbeing. Visit this social page where we focus on areas other than typical dentistry which we believe impacts overall health.
Sleep hygiene
Sleep is an essential part of feeling well and happy, but almost everyone experiences problems sleeping at some time in their life. Sleep disruption is common, especially during times of heightened emotions such as stress. To improve your sleep, try some of the following suggestions which are known as good sleep hygiene:
- Avoid things that give you energy before you go to bed such as caffeine or nicotine.
- Don’t go to bed too late or too tired.
- Improve the quality of your sleep environment. Have a comfortable bed and pillow, in a quiet and darkened room, at a comfortable room temperature for you.
- Consider relaxation and meditation prior to going to sleep.
You may be offered a splint. This helps to protect the teeth for those that grind or clench excessively and makes it harder to clench and grind. However, research is inconclusive for the use of splints to decrease bruxism and TMD.
The role of stress
Stress can prolong jaw muscle pain and potentially make it worse. Treatments focusing on reducing stress may be useful and may also help to reduce your pain. TMD lasting over six months may cause changes in your emotional wellbeing.
The following treatments may be beneficial in improving your wellbeing and reducing stress. Understanding and acknowledging these issues is the first step to improving your chances of a good recovery. Therapies which might help include:
- Relaxation therapies, including relaxation apps such as Calm© or Headspace©
- Abdominal breathing techniques
- Meditative yoga
- Mindfulness techniques
- Talking therapies such as Cognitive Behavioural Therapy (CBT).
References:
- National Institute of Dental and Craniofacial Research: Prevalence of TMJD and its Signs and Symptoms.